
ARE YOU AT RISK OF DIABETES?
BEING A MAN Men may be more likely to develop type 2 diabetes than women. Researchers have discovered that men seem to develop type 2 diabetes at a lower Body Mass Index than women of a similar age. The proposed reasons are that men may be less sensitive to insulin than women or tend to store fat around their organs rather than under the skin as women do.
THE WEIGHT FACTOR
Being overweight (having a Body Mass Index of 30 or greater) puts you at a greater risk of diabetes. It matters where exactly you accumulate your fat. If you store fat mainly in the abdomen, you have a greater risk of type 2 diabetes than if you store fat elsewhere, such as in your hips and thighs. Your risk of type 2 diabetes rises if you are a man with a waist circumference above 36 inches (90) or a woman with a waist that’s greater than 31.5 inches (80). Studies suggest that the more excess weight you have, especially abdominal fat, the more resistant your liver, muscle and tissue cells are to the insulin hormone. This is known as insulin resistance – the hallmark of type 2 diabetes. Implication of this? You can cut your risk of developing type 2 diabetes by losing weight.
ARE YOU ACTIVE?
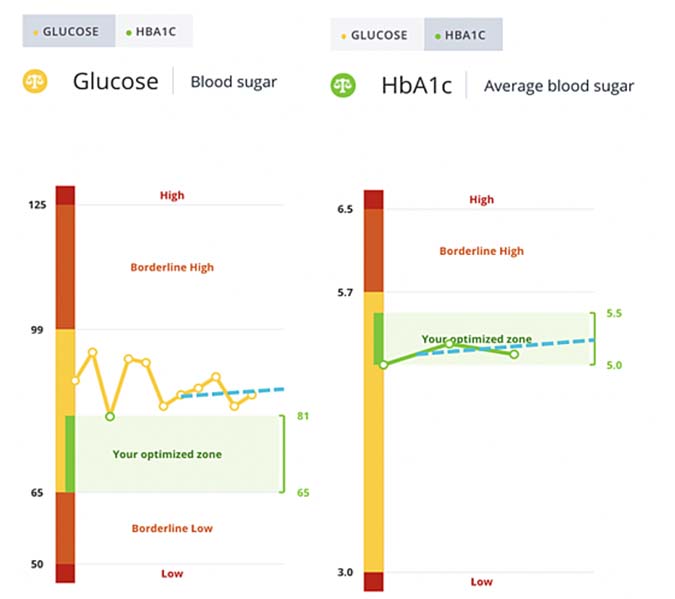
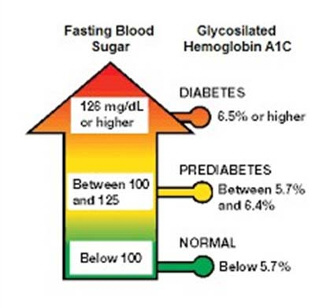
The benefits of physical activity cannot be overstated. In fact, the less active you are, the greater your risk of type 2 diabetes. Many studies underscore how physical activity and exercise help control weight, uses up glucose as energy and make our cells more sensitive to insulin. For instance, exercise has been found to have lower HbA1c value in people with diabetes. (HbA1c test measures the amount of glycosylated hemoglobin or glucose coating around your hemoglobin the blood to indicate how well a person’s diabetes is being controlled over time.) People with diabetes have also been found to have a lower risk of developing heart disease when they walk for at least two and a half an hour (150 minutes) a week. Such benefits persist even with confounding factors, including BMI, smoking, and other heart disease risk factors.
FAMILY HISTORY
Family history of type 2 diabetes is recognized as an important risk factor of the disease. The risk of type 2 diabetes increases if your parent or sibling has type 2 diabetes. In fact, the risk of type 2 diabetes can go up two to six times for them, compared with people with no family history of the disease. The causes of type 2 diabetes are complex: family medical history provides valuable genomic information because it represents the combination of inherited genetic susceptibilities and shared environmental and behavioral factors. The use of family history as part of a comprehensive risk assessment for an individual can be crucial in the prevention, early detection, and treatment of type 2 diabetes.
PREDIABETES FIRST
Prediabetes is a risk factor for diabetes. It is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes. In fact, the complications associated with diabetes are present among people with undiagnosed prediabetes at higher rates than among people with normal glucose levels. Prediabetes is, however, a condition that can mostly be managed with lifestyle changes. With simple changes, such as weight loss, a healthier diet, and getting more active, you can dramatically lower your risk for type 2 diabetes, and improve your health and quality of life at the same time!
HOW OLD ARE YOU?
Age is one of the most important risk factors for type 2 diabetes and the burden of the disease is very high in older age groups. In fact, diabetes is a progressive disease. Glucose levels are known to increase with age. And so does the risk of type 2 diabetes as you get older, especially after age 45. Part of the reason is that, people tend to exercise less, lose muscle mass and gain weight as they age. There is, however, also evidence that diabetes in the elderly may result from an age-related decline in beta cell function. Beta cells are cells found in the pancreas that make the insulin hormone, responsible for controlling the level of glucose in the blood. It is believed that the impaired secretion of insulin from beta cells leads to diabetes in elderly adults.

GESTATIONAL DIABETES
For women, developing diabetes during pregnancy puts one at greater risk of type 2 diabetes. If a baby weighs more than 9 pounds (4 kgs) at birth, the mother is also at risk of type 2 diabetes. New mothers are advised to get tested for diabetes six to 12 weeks after child birth, and to continue to get tested, at least, every two to three years even if found to be normal. They are at the risk of getting diabetes during their entire lifetime. Children of women who had gestational diabetes, are also at risk of getting diabetes. Early detection can help prevent diabetes complications.
POLYCYSTIC OVARIAN SYNDROME
Polycystic ovarian syndrome (PCOS) is a common condition characterized by irregular menstrual periods, excess hair growth and obesity. PCOS involves small cysts forming on the ovaries. These can impair ovulation and fertility. It is related to an imbalance of hormones, including the hormone insulin. A person with PCOS is more likely to have insulin resistance, typical in type 2 diabetes.
SKIN TAGS
A range of skin conditions appear and can be early indicators. Research shows that there is an increased risk of diabetes in people who develop areas of darkened skin (called as acanthosis Nigerians) usually in the armpits and neck, and/ or small growths on the skin that hang from stalks (skin tags). Medically harmless, these conditions often indicate insulin resistance. Reduced sensitivity of nerves and circulation, however, often make it harder to spot emerging skin problems.


Diabetes and brain damage: The wireless connection!
Diabetes Brain Damage, when citing the dangers of Type 2 diabetes, doctors usually focus on associated, life-threatening conditions such as heart disease and risk of stroke along with microvascular complications such as retinopathy, nephropathy, and neuropathy. Research is beginning to show, however, that diabetes brain damage occurs directly—filling in the details of a picture in which insulin resistance, memory loss, and even Alzheimer’s disease are ominously intertwined. While the deleterious effects of diabetes mellitus on the retinal, renal, cardiovascular, and peripheral nervous systems are widely acknowledged, less attention has been given to the effect of diabetes on cognitive function. Both Type 1 and Type 2 diabetes mellitus have been associated with reduced performance on numerous domains of cognitive function.

Life expectancy is increasing, that’s good news. The downside to this trend is that more and more people will develop diseases such as diabetes or Alzheimer’s and some may even be unfortunate to be in a state of ‘buy one – get one’ (diabetes plus Alzheimer’s). In fact, epidemiologic studies have shown having Type 2 diabetes increases the risk of developing Alzheimer’s disease by 65% and that 80% of Alzheimer patients have problems with glycemic control.
Meals, insulin, and brain function:
Within minutes of a meal, insulin is sent to the brain to help neurons absorb and use glucose. Smaller increases in insulin also occur throughout the day, likely in response to neural signals. In the brain, insulin has a number of roles to play. It promotes glucose uptake in the neurons of the hippocampal formation and the frontal lobes, areas that are involved in memory. Insulin also strengthens the synaptic connections between brain cells, helping to form new memories. In addition, insulin regulates the neurotransmitter acetylcholine, which plays an important role in learning and memory. Finally, insulin is involved in blood vessel formation and function.
Brain insulin resistance:
Insulin and related growth proteins in the brain are vital for cell survival, and both glucose and insulin appear to regulate many brain functions, including learning and memory. The dysfunction of these chemicals contributes to cognitive deficits. Chronic episodes of high or low levels of blood glucose may directly affect insulin’s actions in diabetes brain damage or damage brain cells, leading to cognitive impairments. New evidence shows that the insulin-insensitive state found in our liver, fat, and muscle cells/tissues corresponds with insulin sensitivity in our central nervous system as well (insulin resistance at the level of brain). This impacts the areas of the brain responsible for cognition, memory, and learning. Diabetes may be wreaking havoc, especially in the hippocampus. The hypothalamus—a brain region that regulates metabolic processes and activities like hunger, thirst, and body temperature—also appears to be involved, especially areas that respond to low blood sugar and regulate energy balance, body weight, and the sensitivity of the liver and muscles to insulin. Insulin is involved in long-term potentiation, a process of memory formation at the cell level; it also regulates several of the chemical messengers involved in memory, such as acetylcholine. At low doses, insulin helps to contain the inflammation and, at high doses, stimulates it. Increased insulin concentrations also appear to boost levels of beta-amyloid – a protein involved in the formation of senile plaques that can lead to Alzheimer’s disease. Because inflammation, reduced acetylcholine, and toxic accumulations of beta-amyloid protein are hallmarks of Alzheimer’s disease, insulin insensitivity is one route through which this disease may develop.
Those suffering from Type 2 diabetes and insulin resistance also run a heavy risk of developing impaired cognition and increased risk for dementia or memory loss and developing Alzheimer’s disease. Insulin regulates the brain’s supply of dopamine which is a neurotransmitter that helps in attention, reward, and motor activity and any disruption or abnormality in insulin action can lead to brain disorders and cognitive imbalances in mood and disorders like depression, Parkinson’s disease, schizophrenia, and attention-deficit hyperactivity disorder. In the present day digital world, cognitive decline can have very serious consequences because you could forget passwords, secret codes, locker numbers, and bank PINs!
Two-way scientific and treatment benefits:
There is mounting evidence that scientists from the metabolic and central nervous system (CNS) fields must unite and look at neurodegenerative processes from a different angle, taking into account the evidence generated whilst studying metabolic diseases. Conversely, knowledge generated in CNS labs could contribute to innovative ways to prevent and treat metabolic diseases. Here are some questions that scientific brains and hands together address: a) How do metabolic states affect brain function? b) How can CNS targets expressed in the periphery regulate metabolism? and c) How can anti-diabetic compounds contribute to preventing and treating neurodegenerative diseases?
An ‘executive’ could lose executive function:
Since diabetes impairs planning, coordinating, sequencing, and monitoring of cognitive operations, collectively known as ‘executive function’, the so-called ‘business executive’ developing diabetes could end up with the loss of executive function. Therefore, it’s important to prevent cognitive decline. Evidence from neurocognitive testing suggests that cognitive dysfunction should be listed as one of the many complications of diabetes. Recently, it is also emphasized that clinicians should consider cognitive function in assessing and guiding their patients regarding safe diabetes self-management regardless of their glycemic targets. If someone asks what’s special about Diabetes Specialty Centers – the answer is this –holistic treatment beyond just glucose control – where the doctor treats physical, metabolic, mental, psychosocial, and behavioral aspects of the patient. There is good news though! Prevention and even reversal of diabetes and obesity-related cognitive impairment and depressive mood can be brought about by lifestyle modification. Again and again, scientific research and the medical community emphasize the same slogan: ‘prevent and control diabetes with appropriate lifestyle modification and live a healthy life’, the same wine (message) in a new bottle (evidence). The ‘voice’ should now reach beyond ears – right up to the brain for better cognitive function and best quality of life.
Smoking and Diabetes: The Double Health Hazard
Smoking affects all people who smoke. However, for people with another illness, such as diabetes, smoking worsens symptoms and makes the illness harder to manage. India has the second largest population (1210 million) and number of people with diabetes (69 million) and tobacco users (275 million) after China. Both diabetes prevalence and tobacco use are increasing rapidly in India. Smoking is strongly linked to the risk of diabetes, morbidity as well as mortality. The International Diabetes Federation (IDF) in 2003 and the American Diabetes Association (ADA) in 2004 have both strongly recommended that people with diabetes not smoke because of increased risk of diabetes complications.

What do cigarettes contain?
The main ingredient in cigarettes is tobacco. Tobacco is a green, leafy plant that is grown in warm climates. Farmers use many chemicals to grow tobacco. They use fertilizers to make the soil rich and insecticides to kill the insects that eat the tobacco plant. After the tobacco plants are picked, they are dried, and machines break up the leaves into small pieces. Artificial flavors and other chemicals are added. Some chemicals are put in cigarettes to keep them burning, otherwise, they would go out. There are over 4,000 chemicals in cigarettes. 51 of them are known to cause cancer.
Does tobacco increase the risk of diabetes?
Yes. Tobacco can increase blood sugar levels and leads to resistance of insulin in the body. Studies have shown an increase in the occurrence of diabetes among smokers i.e. smokers are three times at more risk of developing diabetes than non-smokers.
Why is smoking particularly bad for people with diabetes?
Diabetes is a chronic disease and if not managed properly can lead to long-term complications such as heart disease, kidney disease (nephropathy), nerve disease (neuropathy), eye disease (retinopathy) and foot disease. Smoking combined with diabetes increases the risk and severity of diabetes complications. Smoking can in fact accelerate the onset of diabetes related complications due to its (damage to the inner lining of blood vessels).
What are the harmful effects of smoking with diabetes?
As smoking increases blood sugar levels, maintaining good blood sugar count can be difficult for smokers. It is clearly established that smoking is a fairly large and independent risk factor for heart disease, stroke and peripheral vascular disease in people with diabetes. Smokers are also more at risk for nerve and kidney damage.
How does smoking increase heart disease risk in people with diabetes?
About 20% of deaths from heart diseases are attributed to smoking. Smoking can damage the lining of the blood vessels and cause the build-up of fatty deposits in the arteries (atherosclerosis). It raises the heart rate and blood pressure by causing narrowing of the blood vessels (vasoconstriction). It increases the likelihood of forming blood clots in the arteries leading to heart attacks. It reduces the flow of oxygen to the heart and damages the heart muscles.
Tips for quitting smoking
Quitting smoking can be difficult, but it is possible. Ex-smokers enjoy a better quality of life, have fewer diseases and an increased lifespan compared to those who continue to smoke.

Here are five simple steps to get started:
• Talk to doctor and create a quit plan. Ask about nicotine replacement therapy (NRT).
• Talk to friends and family about quitting. Ask them for support.
• Never stay bored. Get busy. Try to get out of your home and go for a walk or exercise if you feel alone and bored.
• Avoid people, places, materials and situations that can trigger your urge to smoke.
• Stay positive. Whenever you feel like having your next puff, think about why you quit in the first place. It can be hard but the reward is more than worth it. Doctors are the best people to address your concerns and make further recommendations.
There is no evidence that e-cigarettes are a healthier alternative to smoking. Cessation is the best advice.
Diabetes and Cancer

Key points:
• Diabetes increase mortality in people with cancer.
• Aging, sex, obesity, physical activity, diet, alcohol, and smoking are common risk factors for diabetes and cancer.
• Diabetic patients should have routine screening for cancer.
Both diabetes and cancer are prevalent diseases whose incidence are increasing and have a great impact on the health worldwide. Individuals with diabetes may have an increased risk of cancer. It has been observed that cancer and diabetes are diagnosed within the same individual more frequently than would be expected by chance. Studies suggest that diabetes may significantly increase mortality in people with cancer.
Evidence suggests that people with diabetes are at significantly higher risk for many forms of cancer. Diabetes, predominantly type 2 diabetes (non-insulin-dependent diabetes), has been associated to certain cancers, while prostate cancer occurs less often in men with diabetes. The risk for cancers of the liver, pancreas, and endometrium are about two fold or higher and lesser for cancers of the colon and rectum, breast, and bladder in individuals with diabetes. Other cancers (e.g., lung) are not associated with an increased risk in individuals with diabetes.
About 80% of pancreatic cancer patients have glucose intolerance or frank diabetes. In patients with Type II diabetes, the pancreas is generally exposed to substantial hyperinsulinemia for years, suggesting that insulin may be involved in the association between long-standing diabetes and pancreatic cancer. Recently-developed glucose intolerance or diabetes may be a consequence of pancreatic cancer and that recent onset of glucose intolerance or diabetes may be an early sign of pancreatic cancer.
Type 2 diabetes and cancer share many common risk factors, but potential biologic links between the two diseases are not clear. Potential modifiable and non-modifiable risk factors common to both cancer and diabetes are shown in figure below. In addition, evidence suggests that some medications used to treat hyperglycemia are also associated with either increased or reduced risk of cancer.
Dos and Don’ts in Diabetes
The first line of management of all patients with diabetes is healthy eating and regular physical activity. Medications are second line treatment measures, if diet and exercise fail to achieve adequate control. Medication in diabetes can either be oral tablets (oral hypoglycemic agents or OHAs) or insulin injections. A diabetes person’s diet need not be a complete deviation from the normal diet. The nutritional requirements of a person with diabetes are the same as in the person without diabetes. However, the nutrient intake has to be tailor made based on the age, sex, weight, height, physical activity, physiological needs and current dietary history and routine of the patient. Heathy eating is the corner stone of therapy for diabetes mellitus. An individual with diabetes can often manage his condition by diet and exercise alone. When a patient with diabetes neglects this important aspect of diabetes management, then his/her blood sugars become uncontrolled.
Do’s

Diet plan should be balanced and individualized.
The calculated caloric requirement should allow the patient to lose or gain weight as required and maintain body weight close to the ideal/ desirable body weight.
Restrict refined and starchy food items such as maida, rava, white bread, potatoes, other tubers, processed foods and meats.
Include loads of vegetables and 1 or 2 helpings of fruits such as oranges, papaya, mosambi, guava or watermelon. Sweet tasting fruits need to be restricted; for ex.Sitaphal (custard apple) chickoo, sweet bananas, grapes, mangoes etc..
Include mainly high fiber foods (whole grains, pulses, and all green vegetables).
Daily fiber intake should be at least 20-35 g. Fiber helps to reduce postprandial blood glucose levels and blood cholesterol.
Make greens and vegetables part of your daily diet.
Eat diet low in glycemic index which helps keep the blood sugars in normal range.
Butter, ghee, coconut oil and palm oil are rich in saturated fats and should be restricted.
Mustard oil, corn oil, sunflower oil, groundnut oil, rice bran oil and gingelly oil can be preferred i.e. saturated fats less than 10 percent, monounsaturated fats and polyunsaturated fats in the ratio 1:1 of the remaining fat %. Olive oil best used for salads in cooking. Avoid trans fats such as margarine and dalda/vanaspathi.
Maintain a small food diary. Keep track of all the food you eat in a day. You will be amazed at the amount and type of food you eat.
An obese patient should restrict calories through reduction in the intake of carbohydrate and fat. Ensure that food is eaten not only at the appropriate time but also in appropriate amounts.
Include 4-6 small frequent meals rather than 3- big meals a day.
When you shop, cook or eat out, make healthy choices.
Always read labels and select foods that are low in fat, salt, sugars.
Chew your food well and drink sufficient amount of water.
Try and Include salads in lunch and dinner.
Avoid Table salt and restrict use of processed foods.
Don’t

Patients who are on insulin or oral hypoglycemic agents should not fast, because it may result in hypoglycemia (low blood sugar levels).
They should not skip a meal assuming that it can be made up by consuming extra food at the next meal. This may result in low blood sugar and also blood glucose fluctuations which leads to microvascular complications.
Do not eat white bread, chips, and pastries, which quickly increase blood sugar.
Avoid processed foods and meats as they will be rich in salt and oil.
Restrict fried and fatty foods.
Do not take full fat dairy products.
Alcohol increases blood pressure and triglycerides and heavy drinking weakens the heart muscle (cardiomyopathy). In excess, it affects the liver and peripheral nerves.
Do not use artificial sweeteners beyond the recommended quantity. If possible, get used to tea/coffee without sugar gradually.
Do not exercise on empty or full stomach.
Do not watch TV while eating food.
Do not smoke.
Do not miss your medication.